NPIS Model
In the era of health disinformation
fake medicine, abuse, and sectarian excesses, misinformation in the health field is everywhere (1). The sector of intangible prevention and care solutions is particularly exposed.
But how can it be avoided when the term that describes them conflates discipline, approach, method, and technique (2), when the interventions that claim to be based on them lack a consensual validation framework, when best practices are not shared in a multi-professional repository, when practitioners are accustomed to reinventing their procedures for each new patient, and when researchers underline the inadequacy of their description in scientific articles? (3) This is what happened to NPI, a term used “Non-Pharmacological Intervention” (NPI) has been used by numerous health authorities, including WHO since 2003, the UK's National Institute for Health and Care Excellence (NICE) since 2008, the French Haute Autorité de Santé (HAS) since 2011, the Irish Department of Health since 2014, the US National Institutes of Health (NIH) and the Japanese Ministry of Health, Labour and Welfare since 2016, the Chinese Center for Disease Control and Prevention (CCDCP) since 2017, the Indian Council of Medical Research (ICMR) and the French Ministry of Health since 2018, the European Centre for Disease Prevention and Control (ECDC) since 2020, the Belgian Superior Health Council and the Public Health Agency of Canada since 2021, the European Commission and the Australian Institute of Health and Welfare (AIHW) since 2022, the Organisation for Economic Co-operation and Development (OECD) since 2023, the Swiss Federal Office of Public Health since 2024.
The NPIS co-constructed, with all stakeholders in the ecosystem, a definition, scope, and evaluation framework for these intangible prevention and care solutions (4).
This consensus work was conducted over two years using a rigorous, interdisciplinary, intersectoral, and cross-partisan approach. It brought together more than 1,000 participants. The paradigm was called the NPIS Model (5). A previously dispersed network of stakeholders will be able to better promote their practice through research and science, similar to the drug field some fifty years ago.
A Consensual Definition
An NPI corresponds to an "evidence-based, effective, personalized, non-invasive prevention or care protocol, registered and supervised by a qualified professional" (4).
It aims to prevent, treat, cure, or support a health problem known to evidence-based medicine. The problem may be an illness, a symptom explained by a medical diagnosis, a risk factor, a disability, or an end-of-life period. An NPI is a targeted protocol that must be personalized according to the user and the implementation context. It is offered for a limited period. It can have a leveraging effect by sustainably changing health behaviors (e.g., quitting smoking, using a bicycle for daily travel). It has a dominant physical, nutritional, or psychosocial focus. The physical domain includes, for example, physiotherapy protocols, manual therapies, exercise programs, occupational therapy methods, psychomotor programs, midwifery protocols, nursing protocols, speech therapy methods, horticultural therapies, and thermal treatments. The psychosocial domain includes, for example, psychotherapies, health prevention programs, disease management programs, art therapy protocols, music therapy programs, body-mind protocols, and animal-assisted therapies. The nutritional domain includes, for example, specific diets and intermittent fasting.
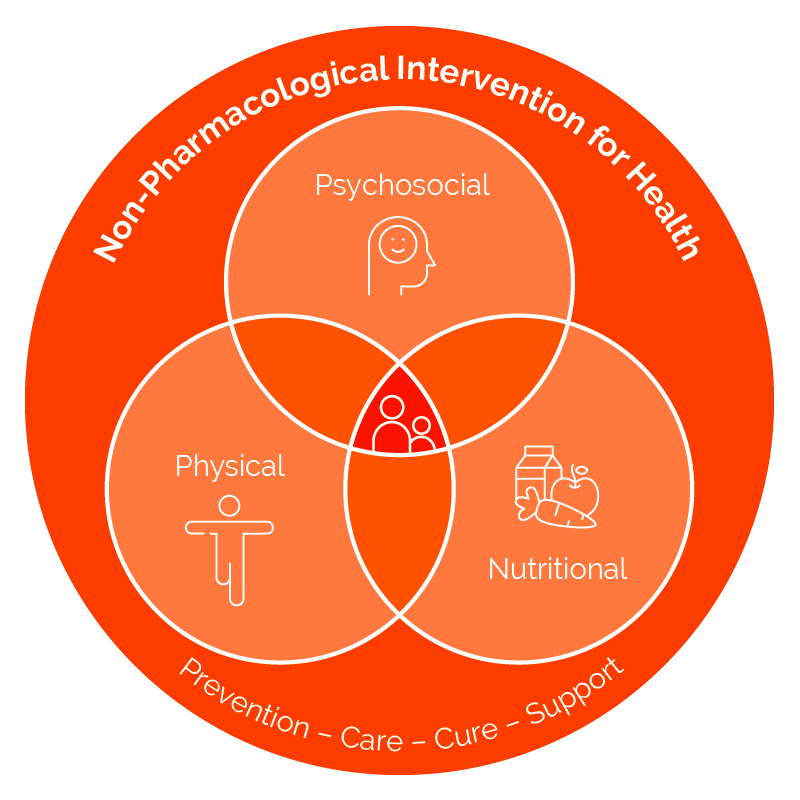
Scope of Non-Pharmacological Interventions in Health
A Harmonized Evaluation Framework
The established evaluation framework is based on international scientific recommendations in the field of health and the patient-centered approach. It recommends 14 ethical invariants and 63 methodological invariants divided into five study types: observational, prototypical, mechanistic, interventional (or clinical), and implementation. This innovation has been presented to all French, European, and international health authorities. The model is now supported by 32 French and European scientific societies, French and European research networks, and French and European user organizations (5).
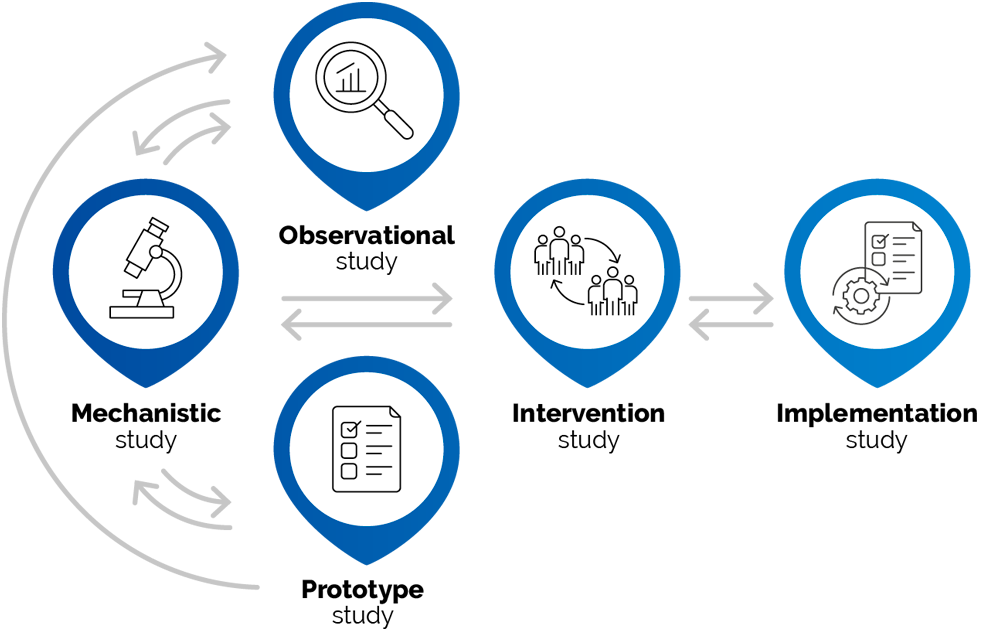
NPIS Model, a consensual scientific framework for developing NPI for health
An open and scalable framework
The evaluative consensus has legitimized the creation in 2024 of an open digital platform of codified, applicable, traceable, fundable, and scalable NPI records. The NPIS has named this library of operational health protocols accessible online, the NPIS Registry.
The NPIS Registry, the repository of open-access NPI card
Each NPI is presented in the form of a practical card intended for the general public and health professionals.
Each card submitted by healthcare professionals has been validated through a rigorous and independent process of scientific expertise, verifiable by all health authorities and scientific societies. The NPI card has received approval from a committee of experts based on five fundamental properties:
- The NPI is described by at least one prototypical study publication highlighting its characteristics (designation, primary benefit, secondary benefits, risks, mechanisms, target population, protocol/program, professional, context of use).
- The NPI is explained by at least one mechanistic study publication highlighting at least one biological mechanism of action or a specific psychological process explaining its effect on the primary health marker described in the WHO 11th classification of diseases.
- The NPI is effective by at least two clinical studies publications demonstrating the reproducibility of its effect on the main health marker in a target population.
- The NPI is safe by the publication of at least two studies publications identifying its risks and precautionary measures.
- The NPI is implementable by at least one implementation study publication determining its deployment, customization, and adaptation to a given territory and cultural context, consistent with the recommendations of health authorities.
The platform collects feedback from patients and professionals to improve the content of NPI card.
The content of each NPIS is shared in a unique card to authors, researchers, scientific society, NPIS partners, and health authorities. The NPIS Registry constitutes a universal repository of essential evidence-based prevention and care protocols. It guarantees their health benefits and minimizes risks. It facilitates their integration into national healthcare organisations, digital systems, and professional training (6). It offers operational solutions expected by personalized and precision medicine. The unique code assigned to each NPI makes them identifiable by AI, which until now only had a number of consultations with a practitioner without details on the content of the service. In France, insurance organizations such as the National Health Insurance Fund, PROBTP, Harmonie Mutuelle, and AG2R la Mondiale, independent living organizations such as the National Solidarity Fund for Autonomy, and social welfare organizations such as the National League Against Cancer support this innovation in favor of more active, sustainable, and equitable human health.
Studies here and there have shown benefits of INM in patients and reductions in treatment and hospitalization costs(6).
The established harmonized scientific framework paves the way for better recognition of these prevention and care practices and the development of a value chain complementary to those of health products, biomedical devices, surgeries, and public health measures (7). An international conference, the NPIS Summit, testifies to this every year. The use of the NPIS Registry will have health benefits: improved health of citizens and caregivers, improved longevity without loss of quality of life, better transferability of practices, coordination of care, prevention, social, and education stakeholders. It will also have social benefits: better recognition of humans who care for humans, reduction of social and territorial inequalities. It will also have economic benefits: improved reimbursements, better traceability, reduction of avoidable health care costs, reduction of the number of biased or unnecessary studies. Finally, it will have positive environmental impacts: more sustainable environment attention and behaviors.
Prescribing an NPI is a way to guide a patient toward an effective, safe, and supervised prevention and treatment practice led by a trained professional, and to be able to discuss the expected/achieved results with them.
The NPIS Model framework is a way to inform patients about the existence of these proven, intangible health practices - in other words, conventional practices. Patients are then free to choose unconventional practices without any liability on the part of the healthcare professional. Every citizen deserves accurate and up-to-date information in this area. This has been achieved. In the health field, this illustrates the famous expression of Albert Camus, Nobel Prize winner for literature: "To misname things is to add to the world's misfortunes. To leave them unnamed is to deny our humanity" (8).
Reference
- The Lancet. Health in the age of disinformation. Lancet. 2025 Jan 18;405(10474):173.
- Majeed A, Abbasi K. Medical journals should use the term "public health and social measures". BMJ. 2025 Mar 4;388:r409.
- Hoffmann TC, Erueti C, Glasziou PP. Poor description of non-pharmacological interventions: analysis of consecutive sample of randomised trials. BMJ. 2013 Sep 10;347:f3755.
- Ninot G, Minet M, Larché J, et al. Interventions non médicamenteuses: un nouveau paradigme et des opportunités pour les internistes. Rev Med Interne. 2025 Apr 26:S0248-8663(25)00535-1.
- Ninot, G., Descamps, E., Achalid, G., et al. The NPIS Model: A Standardized, Consensus-Based Framework for Evaluating Non-Pharmacological Interventions. medRxiv 2025.04.04.25325250.
- Ninot G. Non-Pharmacological Interventions: An Essential Answer to Current Demographic, Health, and Environmental Transitions. Cham : Springer Nature, 2021.
- Minet M, Boussageon R, Coudeyre E, et al. Prescription des interventions non médicamenteuses. Kinésithérapie, la Revue, 2024, 24(270), 37-40.
- Munnich A. Mal nommer les choses. Med Sci (Paris). 2016 Oct;32(10):795-796.
BECOME AN EXPERT IN THE NPIS REGISTRY
All NPI researchers and/or practitioners, as well as user representatives, are invited to submit their application to the NPIS, including a cover letter and CV, by email: